
Um… can I just repeat this: 58% OF UK ADULTS HAVE NEVER HAD AN STI TEST. Really?? This can’t be true, right?
Let’s talk about sex…ually transmitted infections. As possibly one of the biggest taboos and causes of embarrassment with regards to sex and dating, never has it been more important to be able to speak about STIs.
Many issues around this relationship between being sexually active, seeking regular sexual health testing, and being open about sexual past, comes down to one word: taboo. Well, two words if you include ‘judgement’.
Sexual education has come a long way over the years, but the latest findings suggest there’s still a lot of work to be done…
A further 12% of adults haven’t had a test in over 5 years
33% of adults said they never received education about STIs at school
26% of adults revealing that they’d only get an STI test if they experienced symptoms
85% of 53-71-year-olds have never had an STI test
It’s estimated that up to a third of all Britain’s infertility cases are due to the consequences of undiagnosed chlamydia
Almost three in every five Brits (58%) admit they have never had an STI test, with a third (32%) also stating they don’t get tested more frequently because they don’t believe they are ‘at risk from STIs’, according to new research from Medicine Direct.
The survey of 2,368 Brits illustrates that more needs to be done to normalise regular sexual health testing and reduce stigma around STIs amongst adults.
The findings come as part of a campaign called ‘Fruit of Your Loins’, which aims to raise awareness of STI symptoms and increase conversation surrounding STIs – in the hope of reducing the taboo surrounding them. The campaign uses real fruit to simulate STI symptoms in an effort to make them easier to spot and accessible to see.
[Read: STIs Are On The Rise: Check Discreetly With LloydsPharmacy Online Doctor]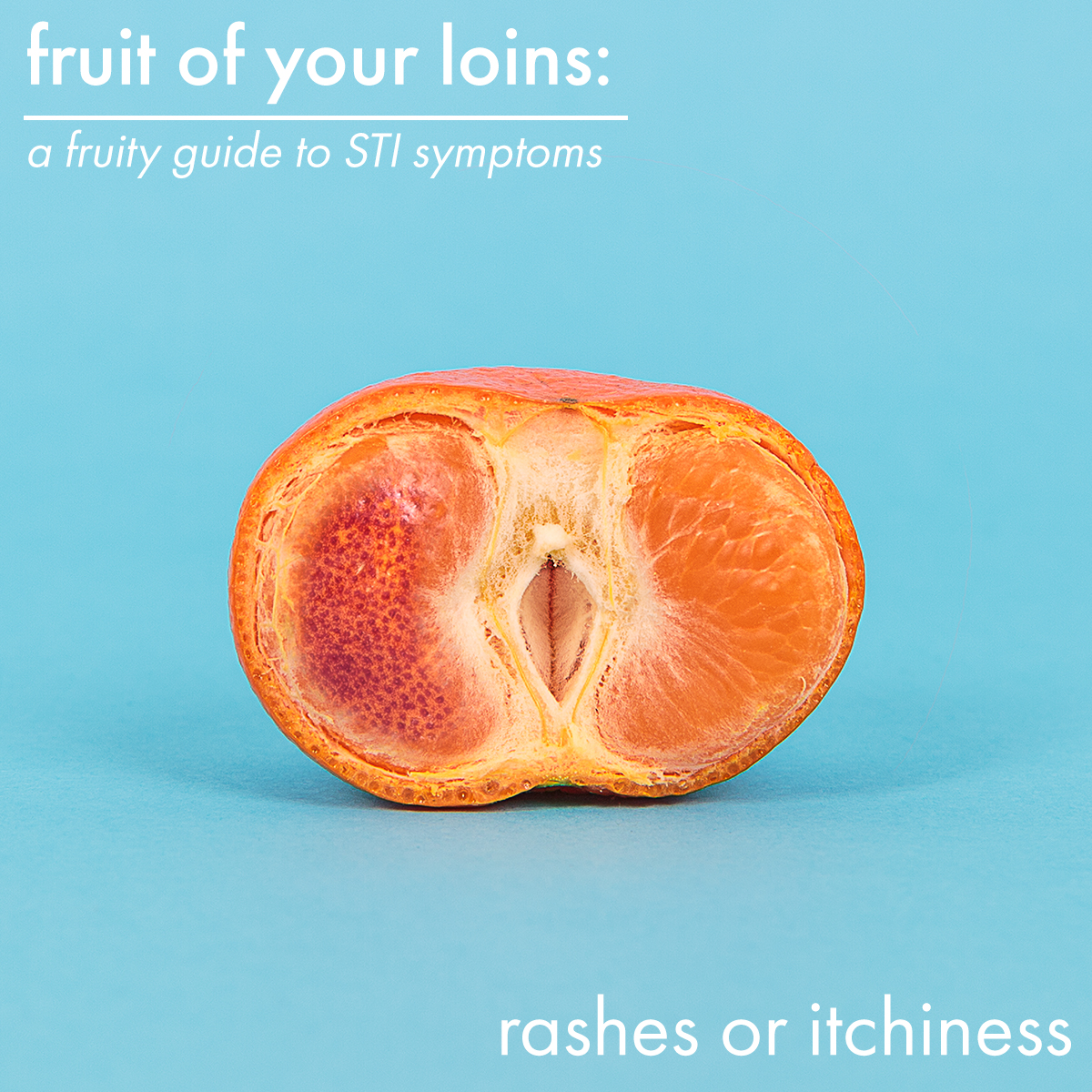
33% of adults said they never received education about STIs at school, and a further 20% found their education about STIs to be poor or awful – highlighting the need for increased focus on positive sexual health routines in sexual education.
Despite there being 422,000 diagnoses of STIs in 2017*, the research also illustrates a lax approach to regular STI testing, with 26% of adults revealing that they’d only get an STI test if they experienced symptoms. This is despite the fact that some STIs, such as Chlamydia, can be largely symptomless and, if left untreated, can lead to reproductive complications and infertility, which is why it’s important to highlight the need to get regular checks and also monitor for symptoms. A further one in ten adults would only get an STI test if their sexual partner told them they had an STI.
Adults also display a reluctance to discuss their sexual history with their partners, with nearly a quarter (23%) stating that they would never feel comfortable discussing their sexual history with their sexual partner.
Other key statistics found in the survey:
- 75% of Edinburgh’s adults and 67% of Glaswegian adults have never had an STI test
- Men were 38% more likely than women to have never had an STI test (69 vs 50%)
- Adults are more likely to turn to Google instead of their partners for advice (11% Google vs 7% partners)
- 18% wouldn’t be confident spotting STI symptoms
- 5% would speak about their sexual history after sleeping together for the first time
- 2% think STIs are a complete myth
Show me the fruit!
Unusual Discharge


Unusual discharge is one of the most common indicators that something’s not right. If you’re experiencing unusual discharge from the vagina, penis or your bottom, it’s time to get tested or talk to a medical professional.
Discharge can take many forms – ranging in colour, odour and frequency – so it’s best to err on the side of caution. If it doesn’t seem within the range of what’s usual for you, get yourself checked out.
Discharge is a symptom most closely associated with chlamydia and gonorrhoea, but there are other STIs that can cause unusual discharge, such as genital herpes and trichomoniasis.
Bacterial Vaginosis is a potential cause of unusual discharge that isn’t sexually transmitted – although it can increase susceptibility to other STIs.
Most causes of discharge can be treated with a short course of antibiotics or, in some cases, a vaginal pessary.
Lumps or skin growths


Skin growths and lumps are symptoms most commonly associated with genital warts, often caused by the human papillomavirus (HPV). If you find yourself with little fleshy lumps and bumps in your genital area, it’s best to speak to a sexual health specialist. Occasionally, these bumps may be textured and rough. They may also be itchy and, in some cases, you may experience bleeding from your genitals or anus.
Treatment can range from a simple cream to a medical specialist physically removing them.
Always seek medical advice if you experience lumps and bumps in the genital area – in rare cases it may be an indicator of cancer.
Rashes or Itchiness


Rashes come in a wide variety of forms and can be indicators of relatively harmless conditions such as yeast infections or more serious concerns such as herpes and syphilis.
Syphilis often appears as small and painless sores, but it is often accompanied by rashes that can appear all over the body, not just the genitals.
As there are so many conditions that exhibit rashes as a symptom, it’s hard to be sure of their cause without seeking medical advice.
Some infections, such as syphilis, won’t go away on their own and can be harmful if left untreated, so it’s important you seek treatment as soon as you notice something’s not right.
Pain When Peeing


If you’re experiencing pain when you pee, you may have a common urinary tract infection (UTI). Whilst these are not necessarily sexually transmitted, they can occur as a result of sexual activity when bacteria from around the genitals can find its way into the pee hole (urethra) and onwards during sex. Most UTIs can pass without antibiotics if you drink lots of water and avoid sexual contact for a week or two.
Painful urination can also be a sign of an STI, such as chlamydia, genital herpes, gonorrhoea, trichomoniasis, or ureaplasma. Chlamydia and gonorrhoea are strongly linked to painful peeing, so if you experience it and have had unprotected sex recently, it’s time to get yourself a testing kit. If you’re diagnosed, you can often be treated with a single dose of antibiotics, so dealing with it is quick and easy.
Blisters or sores


Blisters and sores in your genital area can be quite a shock and should never be ignored. They’re one of the easiest STI symptoms to spot and can be uncomfortable and painful – although just because a sore or blister isn’t painful doesn’t mean it can be ignored!
Herpes, genital warts and gonorrhoea are all major culprits for sores and blisters on the genital and anal area.
With herpes, we can’t currently cure it. You may experience periodic flare-ups that can be worrying, and during this time you might be prescribed anti-viral medication to limit the severity and pain of these flare-ups. It’s totally possible to lead a fulfilling, safe and exciting sex life whilst living with herpes, but it’s important that you’re fully open with any sexual partners that you’re living with the condition.
Gonorrhoea is much more easily treated with antibiotics but (and you may be seeing a theme throughout this article) you should never ignore something that doesn’t look or feel right.
Unusual vaginal bleeding

If you experience vaginal bleeding outside of your normal time window, and you’ve recently had an unprotected sexual experience, you might have an STI.
Chlamydia and gonorrhoea can both cause vaginal bleeding as they cause inflammation and irritation in the uterus (womb), and this symptom can be referred to specifically as pelvic inflammatory disease.
Whilst there are occasions where symptomatic of something relatively harmless, you should always seek medical advice if you are experiencing vaginal bleeding between periods.
It may be an indicator of something that needs treating and can even be an indicator of cancer.
No Symptoms


As we’ve mentioned before, some STIs can exhibit no symptoms. This is why it’s important to work regular sexual health testing into your lifestyle, as sometimes conditions can go under the radar. If left untreated for a long time, it can cause fertility issues for both men and women – it’s estimated that up to a third of all Britain’s infertility cases are due to the consequences of undiagnosed chlamydia.
So what are you waiting for – forget the embarrassment and go book your test now. Infertiliy and further issues aren’t worth being shy for!
Are you worried about your sexual health, or just fancy getting checked? Find your nearest GUM clinic here: https://www.fpa.org.uk/find-a-clinic


